- Bacteriology and Immunology
- Clinical Chemistry
- Medical Genetics
- Pathology
- Virology
- Transplantation Laboratory
- Research Programs
Contact Information
Haartmaninkatu 3 (P.O. Box 21)
FIN-00014 University of Helsinki
Finland
tel. +358 2941 911 (switch)
Background and our previous work (Risto Renkonen Research Group)
Since the beginning of the 1990’s the Renkonen group has focused on the glycobiology of inflammatory diseases and recently began to implement systems biology approaches to this theme.
After thorough evaluation, we have identified type I pollen allergy as a good target to practice systems biology in human patients. Type I hypersensitivity reactions are caused by antigens, such as pollen allergens, which can cross link specific anti-IgE molecules on the presensitized mast cells, where after inflammatory mediators are released, which cause the symptoms of allergy. We focused on this disease because it is common, i.e. up to 15-20 % of the population in Europe suffer from pollen allergies. Allergic symptoms cause a lot of morbidity and thus are a major indirect reason for losses of productivity in the society Furthermore, we can obtain cell and tissue specimens in a time-series manner after allergen challenge both from allergic patients and healthy control subjects and thus hope to collect component data of a dynamic process of a clinically relevant disease, which we will then model by reverse engineering approaches.
Most of the previous work on the pathogenesis of allergies has focused on the mechanisms of the immune responses elicited by the allergen. We have developed an online microscopy allowing us to monitor the real-time development of inflammations in human patients. After showing that birch pollen challenge caused leukocyte extravasation to sites of inflammation within minute, we began to analyze the role of the epithelial barrier in this process. The aim of our systems level analysis is to begin to dissect the role of the first line defense barrier, i.e. respiratory epithelial cells in the early pathogenesis of type I allergic reactions.
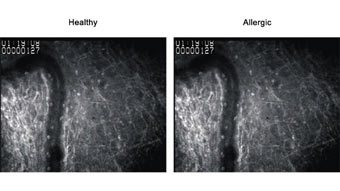
Fig 1. No leukocyte rolling or extravasation seen in conjunctiva of healthy control subjects. However, significant leukocyte rolling and extravasation is present in allergic patients after birch pollen challenge (arrows). A link to the movies »»
Our first results from microscopy, high throughput mass spectrometry and transcriptomics analyses performed with both healthy and allergic subjects, with and without in vivo allergen challenge showed that Bet v 1 binds to epithelial cells within minutes even during asymptomatic winter season, enters epithelium in lipid rafts and caveola and reaches mast cells only in allergic, but not healthy individuals (4, 8, 9). Our first transcriptomics analyses showed that also healthy subjects generate a strong response after challenge with allergens. This response was dominated by transcripts coding for proteins within the immune system (e.g. several chemokines and cytokines). The fact that this immune response is not seen in allergic subjects is of crucial importance. Thus we put out a hypothesis that allergy, at lest for some part, might also be a disease caused by lack of immunoresponses and not only a hyperimmune disease as it has been previously characterized.
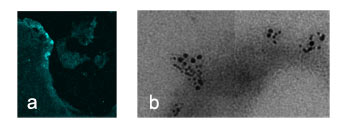
Fig 2. a) Immunohistochemistry indicates Bet v 1 binging to allergic nasal epithelium (blue staining, arrows, magnification x200). Immune electron microscopy shows co-localization of caveolin 2 (5 nm gold particles) and Bet v 1 (10 nm gold particles) on the epithelial surfaces 1 min after in vivo challenge in allergic patients (magnification x100 000).
